December 2022 in England - outcome measures are starting to trickle in
Causal chains, causal chains
I’m not as active on Twitter as I was, but after a quick scan I’ve not yet seen any comment that England’s Ambulance outcome metric data (AmbCO) has reached December 2022.
For anyone wondering why a December 2022 read might be significant, here are the mean times for an ambulance to reach a Category 2 (e.g., a patient with a suspected heart attack or stroke) over the last few years.
Those of us who have been getting somewhat agitated about these times, and pointing out correlations between these measures of response time and unexplained (non-COVID) excess deaths tend to be told (not least by NHS leadership) to sit down and shut up.
For correlation is not causation, and this kind of temporal association is no evidence that it is these long ambulance delays that are are leading to harm. Perhaps the same drivers behind the emergency services pressure are also directly responsible for the excess mortality. For example, the ONS survey revealed simultaneous spikes of flu, RSV and COVID all on top of one another in December 2022, which will have both killed people and also led to increased pressure on the NHS. So, while the ambulance response times will spike up at the same time as excess death spikes, there is a scenario in which the deaths would have occurred anyway, regardless of the delays. Also, it was cold in December. (NHS leadership’s position is that “inclement weather and rising population numbers” may be responsible for the deaths, and that it’s a “huge leap” to suggest that ambulance delays are a major factor).
These updated AmbCO measures cannot directly resolve this question - for the most they can do is show more detailed correlations. But perhaps we can go so far as to claim they are suggestive. AmbCO consist of a bunch of metrics known to to be important to patient outcomes: various milestones timings and rates for stroke, heart attack, sepsis and other urgent conditions.
Let’s start with stroke patients. Here, full outcomes are generally assessed in the long-term and in terms of function recovered by the patient - so these are not yet available (or even defined). But these outcomes are known to be influenced strongly by input measures, such as time between the onset of the stroke to treatment.
As a consequence, anyone who might acknowledge that there is a causal link between time to appropriate treatment for stroke patients and long-term outcomes (e.g., the entire medical profession), a time series like this for the South West region might give a flicker of concern.
The academic literature which brings out the strong link between delays and harms treatment for stroke patient tend to do so in terms of time-to-treatment, not time-to-hospital. So we can add that those patients receiving e.g., thrombolysis generally had to wait a median of ~47 minutes from hospital arrival to treatment. And this doesn’t vary much.
So in December 2022, we could estimate that one in ten stroke patients in the South West face a time between the 999 call and treatment of a bit over eight hours (mean time ~four and a half hours, median around three hours fifteen minutes). I don’t have expertise in this area, but I believe those who do will be looking at these numbers through slits in their fingers.
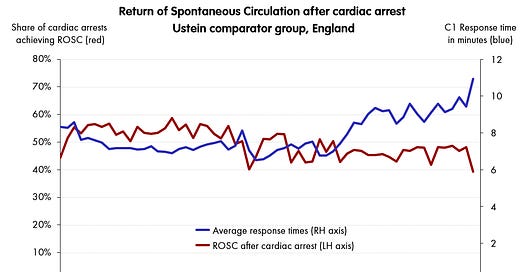
For cardiac arrest, AmbCO goes further and gives time series of selected outcome measures: e.g., whether or not ambulance service can achieve a spontaneous return of circulation in the patient. This is given for various sets of patients including the usefully comparable Utstein group (defined as that subset where the initial arrest was witnessed, with a VF or VT rhythm). Here, I’ve plotted the share of this Utstein group that experienced return of circulation on the same chart as the relevant ambulance response time (C1s for cardiac arrest)
It’s worth mentioning that this ROSC number has been recorded monthly for 12 years now, and December 2022 is the second-worst recorded - you have to go back to the first ever recorded in April 2011, to match it.
Finally, the AmbCO cardiac dataset gives even more direct measures, though only over a shorter period (since 2021). What proportion of various groups of cardiac arrest patients survive to 30 days?
Here, the December 2022 survival figure of 5.3% of all arrest patients (and 19% of Utstein arrest patients) surviving to 30 days are both absolutely the worst ever recorded, though in this case the history is much shorter.
The NHS position remains - as far as I know - that all of this data is irrelevant, since it may be simply be showing spurious correlation. And this is true, it might be that in December the ambulance service were attending to a particularly serious set of cardiac patients - perhaps exacerbated by the COVID, flu and RSV rates - and the longer time they took to get to them, played no causal role in the observation that their survival rates were half of what they were 18 months earlier.
One issue I have with this response (I do have several) is that given the top-level aggregation of the data released publicly, it is always possible to maintain some version of this position. True, you may sometimes look absurd as people dig more and more into the plausible causal chains, but it’s always logically possible.
An additional frustration is that the NHS leadership and analysts have all the non-public patient-level data necessary to split out confounding effects, and reveal the effects of emergency care delays. In fact, they themselves acknowledge both that they have this data, and they claim that they are doing this analysis. Properly.
"We won't know [if delays at A&E are causing the excess deaths] that until we've done the detailed work, which we're in the process of doing."
This is good. This is important. With the patient-level data, you can work out the effects of other factors such as COVID sequelae, such as lockdown health effects, alongside emergency care pressure, and see which ones can be addressed. And with ~80-100 unexplained excess deaths per day, it’s urgent to get it right and start saving lives.
But they claimed this more than five months ago, and since then … nothing.