When all you've got is a sledgehammer, everything looks like a mixed metaphor
Hospitalisation rates from Bayesian Structural Time Series
If you’ve set up an ridiculously overpowered model set to find infection fatality rates from the matchless ONS infection rates and deaths recorded on death certificates, one might ask; “Why not use the hospitalisation data instead, and find infection hospitalisation rates?”
The boring answer to that “why not” is because it’s fiddly. The hospitalisation data is NHS data (not ONS), has a load of “unknown” ages, and every study (even in the same agency) has decided to use different age-groupings to one other. But let’s just cope with that as best we can.1
For details of what we’re up to, please read the previous post, but in a nutshell, we’re using a load of over-specified maths to discover the link between infections in the population and - now - the hospitalisation rates.
That is, if we have a simple relationship:
COVID hospitalisations after some lag = [some number that varies over time] x infections
… then what we’re doing is specifying a model to try to uncover how that number varies over time - it has been chosen to give an estimate of the Infection Hospitalisation Rate (IHR).
It’s harder this time
The main added interest here as compared to deaths is that the lags make an even vaster difference to hospitalisation rates than they do for deaths2 - and can give bizarre effects when peaks are offset from one another. Worse, there was a period - just after the vaccines were introduced in 2021, when hospitalisations plummeted AND the lag between infections and hospitalisations changes.
You can see what I mean from this plot of all ages. Look at the peak of December 2020-Jan 2021: the incidence-to-hospitalisation lag visible in the peaks is around 28 days. It shortens to about 15 days during 2021, and then is down at ~7 days by the time we get Omicron.
For simplicity, I’m going to impose a constant “best compromise” lag throughout, but we still run the risk of weird offsetting effects in some ages, particularly in the middle of 2021, when hospitalisation rates are so low (single figures per day in several age-groups).
We promptly break the whole model
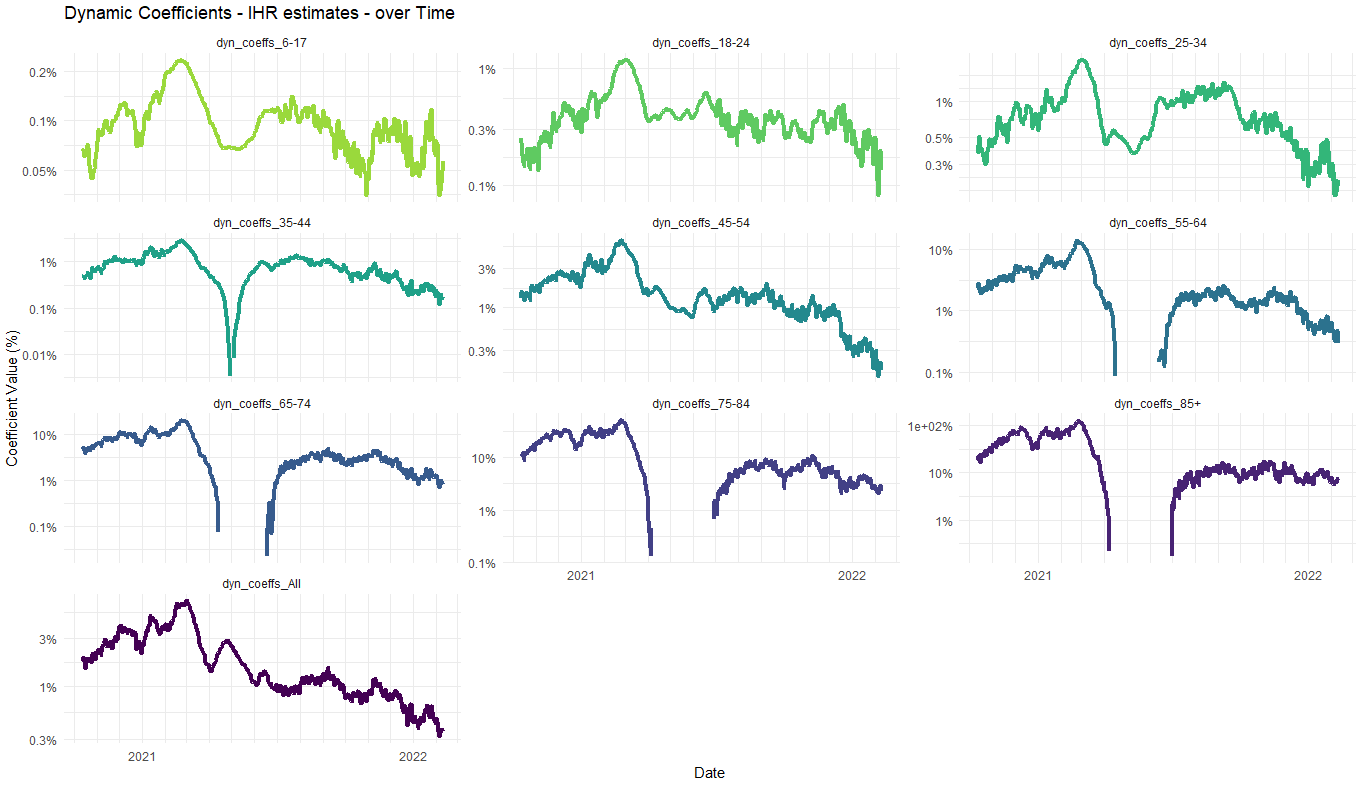
Anyway, pile it all in, and you get this (note the log scale) What’s quite interesting to watch is that how something in the spring of 2021 has such a dramatic effect that it abruptly breaks the model for ages 55 up. That is, this “something” pushes down hospitalisation rates so far and fast, the model simply gives up and thinks that the IHR has gone to zero - i.e., that is there is no link between new infections and new hospitalisations any more.3 Subsequently, more vaccine-evasive and nastier variants like Delta come along later in the summer and edge the hospitalisations back to reasonable levels again, whereupon the model rediscovers the link. Over time, this then diminishes to very low levels as boosters and Omicron comes in (easiest to see this in the 45-54 year olds in “All ages”, at the bottom).
The “All” ages model does a good job of smoothing through most of this excitement and shows quite clearly how we started with an IHR which built a bit, but was building to ~3% and above in December 2020, and then plummeted to its current number value around a tenth of that.
In fact, this headline understates the effect quite a bit - when the time series started, around 80% of the people in hospital with COVID were there primarily as a result of their COVID (as judged by the attending physician). This dropped dramatically as Omicron came in, and is now stable around 30%.
So in terms of COVID actually putting people in hospital (rather than infecting them when there for something else) we’re talking about a factor of 20-30x lower than it was at the end of 2020.
And our survey says …
This is nice of course, but it’s all backward-looking, and raking over some history many are understandably not keen to revisit. However, it also contains a point that might well become relevant shortly.
As we look at hospitalisations right now, in 2023, we are seeing them well below previous pandemic levels, and many people have suggested that this is not real. That the numbers might lower just because we are missing cases in hospitals, due to the far more lax regimes of testing that have come in through 2022 and 2023.
I don’t buy this (and explain why here), but in a few weeks, we should get the chance to check it. This check involves a shed-load of assumptions, but honestly, what’s new?
Our largest assumption is that we should expect IHRs to be roughly where they were at the end of our time series above - variants and boosters have been engaging in a bit of a race, and seem to have come to a stalemate. We should expect all-age IHRs to be bobbing around 0.3%, or 0.1% for “primarily for” COVID.
If so, this gives us a prediction for where the new - more limited - ONS seasonal infection survey might come out for October/November. At the moment, we are at the order of 400 hospitalisation a day with COVID (or about 130 primarily due to COVID). If these rations have remained around the same, so we should expect our survey to tell us that we have around 150,000 new COVID infections a day. Finally, we note that the new survey is far more likely to give us prevalence than incidence (how many infections, not how many new ones) and finally come to the answer that we should be looking at a prevalence number somewhere around 1-2 million for England - around 2-3%. If the hospitalisation rate falls, this number falls too of course, but we can try to match the timing as best we can.4
Much higher than 2-3% (say into double figures on prevalence) would be good prima facie evidence that we are indeed missing a lot of hospitalised cases. Or, lower than this would be good evidence that we were picking them up, but also that the infection hospitalisation rate had decreased since the early days of 2022.
Hospitalisations go up and down faster than deaths, so getting the lag wrong makes things wronger.
Notably, there is no such “breakage” of the model in younger ages, where the vaccine had a much lower take-up or was not offered at all until later on.
In fact, we can get a similar number much more directly, by working directly with ONS prevalence and hospitalisation rates (rather than taking a diversion through incidence). This will remove a lot of the assumptions we have had to make and will be a better indicator. If I have time, I will try to get that estimate before we get the results of the seasonal infection survey.




Soooo good